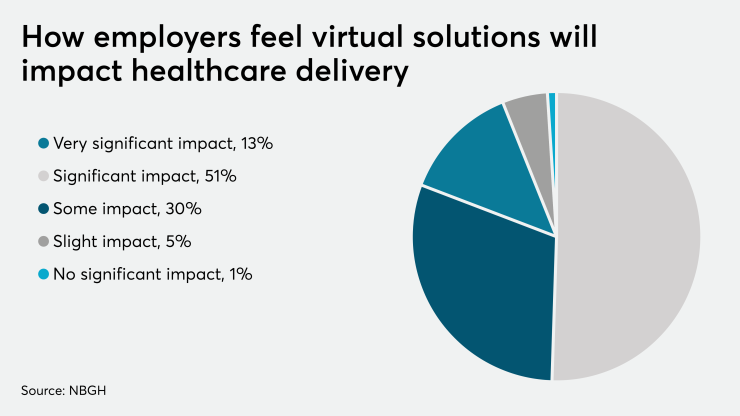
Most employers agree — a more convenient, digital approach is required to
But with seemingly countless patient engagement point solutions on the market, how can your client meet the diverse needs of your employees without overwhelming them with apps, platforms and programs to manage — especially those managing one or more conditions?
And how can the burden be lightened for the employer benefits team, which is faced with the time-consuming responsibility of sourcing and managing numerous vendors across health and wellness, disease-specific interventions and care navigation support.
A new approach being offered by progressive health plans — digital health management — lightens the load of employer benefits leaders while delivering enhanced employee experience and outcomes. Employers who partner with progressive health plans rather than managing numerous outsourced services and vendors, which only address slivers of health management, can stay competitive in a tight job market, control costs and orient employees toward better health by delivering the following capabilities.
Benefits leaders looking to achieve digital health management success should consider health plans that can:
· Help employees better navigate the health system.
· Meet employees where they are.
· Support the whole person to get better results.
Help employees better navigate the health system
More than 80% of employees who can easily access their benefits said they feel loyal to their employer, according to a Thomsons Online Benefits Global Employee Benefits Watch report. But achieving that goal is a complex task. Given the complexities of the healthcare system, it can be challenging to schedule appointments, get financial and administrative questions answered, get support for chronic conditions or guidance following a hospital discharge. As a result, employees may postpone care, make choices that are not cost-effective and feel frustrated with their benefits package.
Also see:
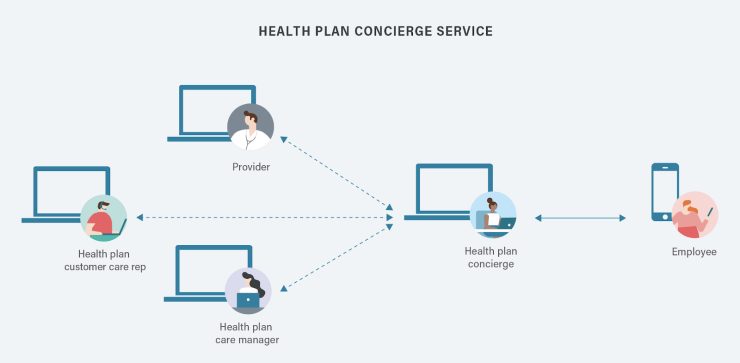
One way to reduce employee frustration and help them better understand and utilize their benefits is to work with health insurers to implement a coordinated and unified concierge service. Such services are accessible by mobile app and provide your employees with a single resource to address their diverse needs. The concierge can develop a trusting relationship with the employee and to help match them to appropriate healthcare resources, whether accessing urgent care, finding a specialist, getting to an appointment or more.
Health plans with digital concierges are also able to integrate the workflows of care management and customer service, which gives them the ability to capture key metrics on consumer actions. The result? Your organization can better forecast what employees need. And with reviews employees may opt to provide through surveys, a forum for data exchange is created that empowers them to better control their healthcare. These new functions can create a quantifiable shift in how employees feel about the management of their healthcare.
In addition to these benefits the digital concierge provides a scalable way to engage more employees, while giving them options to get support through their preferred communication channel. Instead of overwhelming your employees with health communications and outreach, the concierge helps streamline outreach from providers, the health plan, and your third-party services to deliver a better experience. Progressive health plans are starting to segment and target employees not by claim group but rather by social and behavioral conditions. This approach, combined with a new recruitment strategy to engage members, can lead to higher adoption rates and greater employee satisfaction in the long run.
Meet employees where they are
Employees need accessible, and personalized ways to manage their health. These strategies can ensure your health plan offers an experience that drives employee engagement and satisfaction.
Deliver omnichannel engagement: No one likes playing phone tag. That’s why employers should expect health plans to provide health management support through a combination of phone calls, messaging, apps, websites, email and video chat, giving your employees the opportunity choose the method that meets their needs in the moment. Mobile messaging, in particular, ensures flexibility and accessibility, so your employees can respond on their own time, rather than during business hours.
Provide a personalized experience: Avoid a one-size-fits all approach to patient education. Instead, make sure your health plan can deliver dynamic, adaptable health programs with videos, digestible articles, reminders and more health guidance designed to suit the individual needs of each employee.
Build trusted, supportive relationships: An effective health management solution should give employees daily, long-term support from real clinicians, rather than intermittent outreach. Your organization should also consider utilizing a non-clinical engagement specialist, also known as a health advocate, to offer ongoing emotional support and encouragement through mobile messaging. The health advocate can work with the employee over time to set and track progress toward specific, measurable actionable, relevant and time-bound (SMART) goals.
Support the whole person
It’s estimated that most health outcomes are determined by non-medical factors such as behavior, environment, and socioeconomics.
In other words, your employees’ health happens at home.
Also see:
In an attempt to address this, many organizations employ a number of standalone point solutions, such as wellness programs, texting services or condition-specific apps like diabetes programs. According to a Wellframe survey, on average, organizations manage between four and nine different digital point solutions. But instead of helping employees reach their health goals, this approach risks leaving them overwhelmed or confused by often overlapping services.
To improve your employees’ experience, reduce absenteeism and differentiate your benefits package, make sure your health plan delivers holistic support that encourages employees to adopt a new perspective on all the factors that contribute to their health.
Support multiple conditions in a single solution: One in four Americans has multiple chronic conditions, according to the CDC. But most condition-specific point solutions, such as diabetes apps, can’t address the overlapping symptoms your employees may experience. Make sure your health plan offers support for multiple conditions in one solution for conditions like diabetes, hypertension, as well as transitional care.
Address mental and physical health: People with a medical illness or condition are more likely to suffer from depression but the reverse is also true: Anxiety and depression are risk factors for other illnesses, and drive higher incidences of heart disease, diabetes, stroke and other conditions. To support your employees’ whole-health needs, it’s crucial to deliver behavioral health support alongside condition-related guidance.
Reinforce lifestyle changes: To meet their health goals, most employees also need support for weight loss, nutrition and exercise — tangible lifestyle factors they can meaningfully change to improve their health. Providing useful information to help them shop for healthy foods, track their physical activity, for instance, within the context of their clinical condition, will help employees understand how therapeutic lifestyle changes can effect a positive, direct impact on their health.
Your organization shouldn’t have to bear the burden of. Instead, employers should demand more from their health plan partners, who are in the best position to deliver these solutions in a holistic and integrated fashion.