Employers are taking a bigger role in combating addiction problems — working with vendors and ramping up education efforts — to help lessen the impact of opioids in the workplace.
More than half of employers (60%) say they’ve been affected by at least one case of
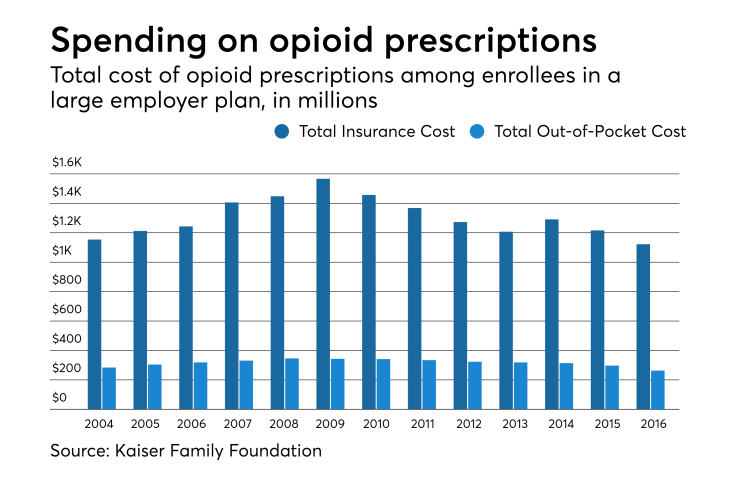
And those impacts are coming at a significant cost, Cheryl Larson, president and CEO of the Midwest Business Group on Health said on a webinar panel Wednesday. Opioid abusers cost employers nearly twice as much ($19,450) in medical expenses on average annually than non-abusers ($10,853).
That’s why companies, including The Boeing Company, are facing the problem head on.
Jason Parrott, manager of healthcare strategy and policy at The Boeing Company, says his company takes a high-profile approach to combating the epidemic — and has for the last several years. Starting in 2015, the aerospace manufacturer began an educational pilot program, mailing letters to patients who were prescribed addictive medications for the first time, as well as the prescribing physicians, alerting them to the risks of the particular drug.
“It was fascinating to see how, on one hand, our members may not have realized the actual risks involved with that prescription medication,” he said. “On the other hand, the prescribing physicians demonstrated a willingness to ratchet back on the day’s supply of opioids they had originally written out.”
In just that pilot alone, after 12 months, Parrott noted the company saw a 30% reduction in the average of days supplied by physicians.
See also:
But that was just the beginning. More recently, Boeing has taken a more holistic view of where access to the medication would come from, Parrott said.
“We started with our pharmacy benefit manager, but then we morphed and looked to our dental plan administrators, behavioral health plan administrators and medical plan administrators, to [identify] the access they bring to the table,” he said.
“One thing that was very striking to me, that I had no idea until we went down this path, dentists write 31% of opioid prescriptions for patients between 10 and 19,” he said.
“We’re really looking forward to understanding how we can improve that [statistic], because clearly, based on some overall research, that’s a huge opportunity for all of us.”
Another change the company made was to carve behavioral health into the medical plan administrator to put it all under one roof.
“For the first time, we have full visibility with both the medical channel and behavioral health channel on what’s really going on to remove those blind spots,” he said.
Looking at these programs from a holistic benefits strategy perspective was key, he said. “It takes a great deal of assessment and analytics and a great deal of collaboration, both internally and with the supply chain.”





