As Congress moves to repeal and replace the Affordable Care Act, details of the new plan are still coming together. Meanwhile, one element appears to have the support of several architects of the various alternative plans that are being proposed by Congress: An expanded use of health savings accounts.
Republicans are pushing for HSA expansion to include greater portability between insurance plans, an increased role for spouses and a raise in the amount that plan participants are allowed to invest. These elements appear in proposals put forth by Speaker Paul Ryan (R-Wis.), HHS Sec. Tom Price’s plan when he was a member of Congress last year, and in a new plan proposed by the Freedom Caucus — led by Sen. Paul Rand (R-Ky.) and Rep. Mark Sanford (R-S.C.).
With the role of HSAs becoming increasingly important in benefit plans, advisers must prepare for how they will handle expanding participation and how they interact with and educate employees on HSAs.
“The Republicans’ plan is more of an expansion of the HSAs. Creating greater rules around those HSAs allows greater portability, more participation with spouses and more protection from bankruptcy. It puts more focus on the participants and less on the employer. It's not so much a new role as more an expanded and just wider adoption,” says Harrison Stone, general counsel at healthcare solutions provider ConnectYourCare, which is based in Baltimore.
By boosting HSAs under the upcoming Republican plan, the end user will have more control over healthcare spending. “The theory is that all of these consumer-owned and directed accounts are empowering. They fit with overall transparency and should force the market to change as providers are forced to more directly compete,” says Dennis Fiszer, first vice president and chief compliance officer for HUB International.
This could downplay the role of employers as employees have a greater say in the way their funds for medical expenses are spent.
“The HSA portion of the account really belongs to the individual. And so, apart from generalized information, the plan sponsor’s role is more hands off … similar to operation of 401(k) programs. The plan sponsor role is focused on operating and maintaining compliance for the accompanying high-deductible health plan. The employer absorbs all the traditional ERISA, COBRA, HIPAA-borne obligations through sponsorship of the HDHP,” says Fiszer.
HSAs by the numbers
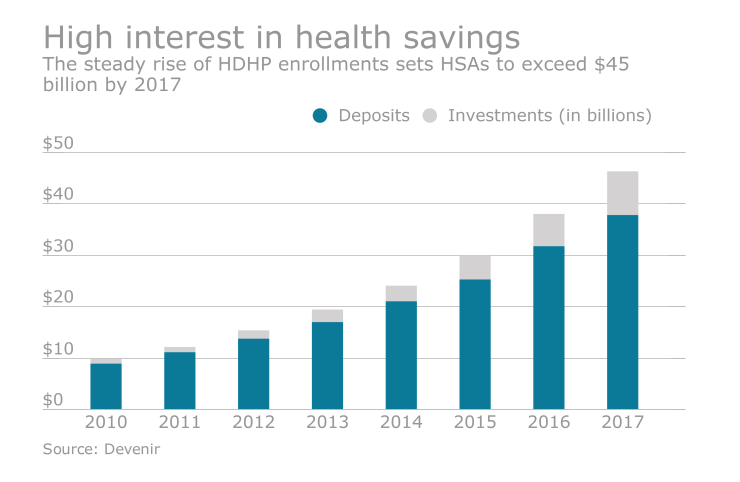
More than 20 million Americans participated in an HSA in 2016, according to America’s Health Insurance Plans. And those numbers are set to climb.
Over the last decade, AHIP found that HSA participation has grown from 3.2 million in 2006 to 20.2 million in 2016. On average, plans surveyed in 2015 and 2016 enrolled an additional 648,000 consumers, which is an average net increase in HSA participants of 3.4%.
HSA adoption is set to take off, says John Young, senior vice president of consumerism and strategy of Alegeus.

Where does Donald J. Trump stand on parental leave, minimum wage and other important workplace issues? Here’s what employers need to know.
“HSAs are at a tipping point for market adoption and have become a foundational pillar for the future success of healthcare, much like 401(k)s are for retirement spending and saving. HSAs are not the panacea to fix all ACA criticisms, but they are a key component of every GOP healthcare proposal,” says Young.
“Simple fixes to HSA accessibility, such as expanded availability to those receiving care under the VA/TRICARE and Indian Health Services, will enable more Americans to have the option of an HSA. Expanding HSA operability, such as increasing contribution limits up to the annual maximum out-of-pocket limit, and allowing spouses to make catch-up contributions to the same account, make HSAs easier to use and understand,” says Young.
Building a smarter healthcare consumer
Ultimately, Republican politicians hope that an expanded HSA will drive down costs as employees search for better bargains in their healthcare. Rand and Sanford’s plan, for example, would sever health insurance from a person’s employer and offer a $5,000 tax credit to fund HSAs.
“What if 30% of the public had health savings accounts?” Paul told
This supposed HSA benefit will require greater data transparency among healthcare providers and advisers, as well as more interaction with plan participants, the employees.
“For this to work the way I think Congress would like it to work is we need greater transparency and [to] know what certain elements of healthcare costs. This country is kind of edging in that direction,” says Edward Fensholt of Lockton Company’s Lockton Benefit Group.
If an employee has a high deductible plan that is supplemented by an HSA, the theory is they would shop for the cheapest medical test or procedure, such as an MRI. In order to accomplish this, the plan participant will need more data from brokers and healthcare providers.
“That data is hard to come by,” says Fensholt. He adds that this proving this information to the plan sponsor is the role of the broker today — and that arrangement will likely have to change.
“Brokers are the ones helping employers drive the market toward that transparency and brokers are developing tools for this. There are some vendors out there that survey the market and sell their data to brokers or to employers as a positive add-on. I think this is all part of a larger theme as in, ‘Let's put employees into more control and more responsibility to manage their healthcare.’”
Although HSAs came into existence in 2004 during the tax reforms of President George W. Bush, there is still
There is risk of HSAs overshadowing other important forms of CDH accounts like FSAs and HRAs, says Young. He adds that “while HSAs are a powerful tool, they are not the end-all-be-all and should not be positioned as such. FSAs and HRAs continue to have an important place in the market.”
As HSAs expand, Young believes that the industry needs to “laser-focus” on consumer education around healthcare consumerism in general and how to maximize the value of all health benefit account offerings. “Without such consumer education, these plans won’t achieve the optimal objective, to lower healthcare costs and improve health,” he says.





