The topic of mental health in the workplace is increasingly becoming a focal point of conversations in C-suites around the country, and rightfully so.
Mental health concerns such as depression and anxiety have a direct impact on an employer’s healthcare costs and their investment in human capital. More than 26% of American adults suffer from a diagnosable mental illness every year, according to the National Institute of Mental Health. And that figure doesn’t include those who are distracted or unproductive at work due to a lower-acuity issue like a relationship problem or job-related stress.
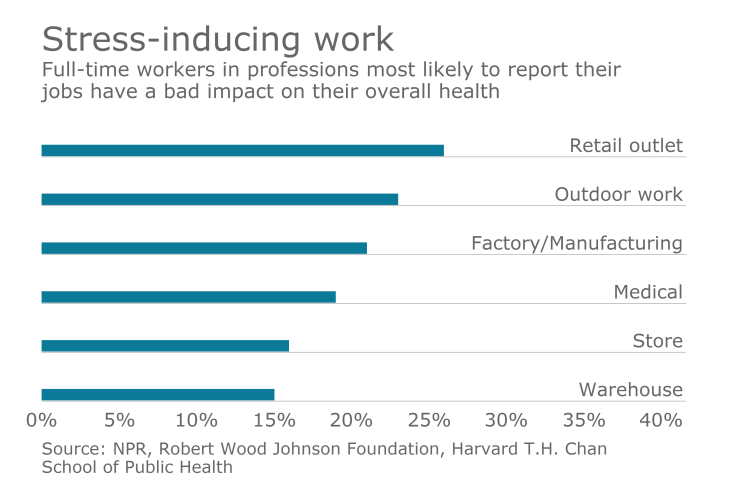
Speaking of stress, the report
These issues are taking a measurable toll on American businesses:
- The CDC reports that the annual direct and indirect costs of treating mental health disorders is $317.5 billion — even higher than the $310 billion OSHA attributes to the annual cost of workplace injuries.
- More workdays are lost or disrupted by mental illness than by chronic conditions such as arthritis, diabetes and heart disease. In fact, employers spend $70 billion each year on lost productivity and increased absenteeism due to untreated or ineffectively treated mental health disorders.
- Depression alone causes an estimated 200 million lost workdays each year and costs employers up to $44 billion annually. In just a three-month period, employees with depression miss an average of 4.8 workdays and 11.5 days of reduced productivity.
- The American Institute of Stress estimates that one million workers miss work each day because of stress, costing companies roughly $602 per employee per year.
Executive awakening
Statistics such as these have led to an awakening at the executive level. With a deeper understanding of the negative impact that mental health concerns have on their company’s bottom line, an increasing number of executives are focusing on mental health as a critical component of their population health management strategies. As a result, this trend has spawned an increase of products and services:
- Teletherapy: Distance (video, telephonic and chat-based) counseling is appealing to individuals in rural areas, to those with mobility problems and to people who simply don’t have the time to visit a therapist in person.
- Computerized cognitive behavioral therapy (cCBT): cCBT, which increases accessibility to therapy through digital platforms, has been around for years, but is going through a technology-fueled renaissance as employers are looking for new ways to engage employees with mental health resources.
- Wellness: Some wellness programs are beginning to provide resources to address stress, anxiety or depression identified during a health assessment. In addition, wellness coaches are being trained to refer participants with comorbid mental health concerns to external programs.
- Self-help video libraries: Once considered too static, certain evidence-based courses are gaining in popularity as users are becoming more empowered to seek care on their own.
There’s no doubt that each of these products and concepts can be effective at extending the footprint of mental health resources and appealing to a portion of an employee population who may not have otherwise sought treatment. However, some employers don’t realize that their EAP likely includes these features already.
An analysis of 3,497 EAP cases in 2016, first during the initial clinical assessment and again after treatment was completed, revealed the following health and productivity-related outcomes:
- EAPs reduce unscheduled employee absences. The average time away from work that was caused by the employee’s mental or emotional health concern(s) decreased by 6.8 hours after using the EAP.
- From among employees who missed at least 20 hours of work due to their presenting concern(s) before using the EAP, the average improvement was 34.4 hours per employee.
- EAPs have a positive and measurable impact on employee productivity. The average ‘presenteeism’ index score increased from 19.9 (moderate productivity) to 24.5 (high productivity).
- 80.8% of EAP participants reported high productivity after utilizing the EAP, compared to just 52.2% prior to using the program.
- EAPs provide care and support for employees with depression. 85.7% of EAP participants who presented with severe or moderately severe depression migrated into minimal, mild or moderate categories.
- 90.1% of EAP participants with depression showed significant (55.7%) or moderate (34.4%) improvement after using the EAP.
- The average AUDIT-C (alcohol use index) score for EAP participants who presented with alcohol use or abuse improved from 6.5 to 3.9 — a significant reduction in the use and abuse of alcohol.
There’s no denying that ignoring employees’ mental health and wellbeing is costly in terms of lost productivity, higher absenteeism, lower employee engagement and increased healthcare and disability costs. Offerings from health management and technology providers can serve as vehicles to drive incremental engagement with the one benefit that has proven to fill the gap of mental health that exists within most employers’ population health management strategies: an employee assistance program.





