Employee benefits are an important part of recruiting and retaining talent and most plan sponsors offer a range of benefits, including medical, pharmacy, behavioral health, dental, vision, disability and life. A common industry practice has been to offer each of these benefits as a standalone product, but this creates a disconnected picture of the whole person’s health and can lead to gaps in care and delays in diagnosis and treatment.
Recently, however, more employers are rethinking how they can package and integrate their benefits to make them not only more attractive, but work better and keep their employees healthier. Additionally, integration helps by simplifying the consumer experience, while reducing the cost of care.
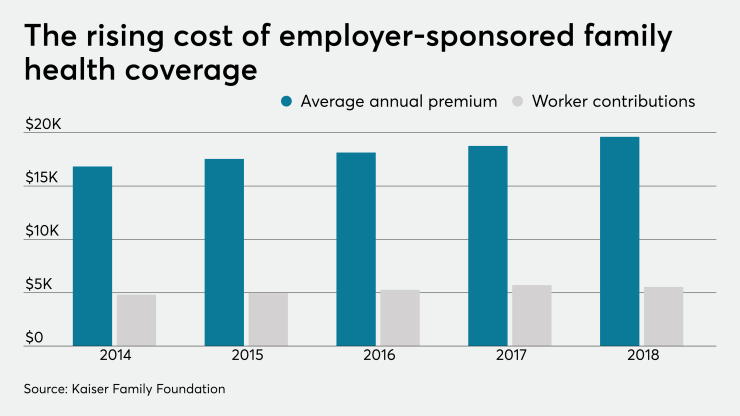
Keeping employees healthy is key to a company’s ability to operate their business, retain stability of their workforce and reduce healthcare costs. For example, absenteeism is a major source of lost productivity and revenue for employers, costing about $226 billion per year, according to the Society for Human Resource Management. When absenteeism is coupled with rising healthcare costs for employers and consumers alike, it becomes clear that preventative treatment and early diagnosis is vital. When healthcare benefits are integrated and coordinated to treat the whole person, it can improve employees’ health by identifying and closing gaps in care and help them get back to work sooner.
Many employers already recognize the value of integrating their health benefit plans. According to a recent study conducted by Anthem, 71% of employers surveyed are either actively integrating or considering integrating their medical, vision, dental, pharmacy, and/or disability benefits in the next five years — this represents an 11% increase from data collected in 2016. The study also found that among those surveyed who are actively integrating or considering integrating benefits nearly 100% of them reported integrating medical plans with pharmacy, vision, dental, and/or disability benefits and the overwhelming preference is for integration with a single insurance carrier versus multiple carriers.
When all of the patient’s medical practitioners, including dentists and optometrists, have access to their relevant health history, providers can co-manage chronic conditions, increase early detection capabilities and coordinate with other providers.
Also see:
For example, if a patient is taking a medication for diabetes that causes dry mouth and forgets to mention it to their dentist, the dentist can access their medical claims to see the patient’s prescription history and take preventative action before further dental issues occur. This provides a fuller picture of an employee’s medical history.
Integrating health data can also simplify and safeguard patient care to prevent complications. If your employee can’t remember the name of a medication they’re currently taking, it can create confusion for their doctor, particularly since two similar-sounding medications can do very different things and require very different advice. Imagine a scenario where an employee is taking two different medications for two different conditions, unknowingly putting themselves in a situation where the treatment for either or both no longer work, or worse, are contraindicated.
This disconnect can cause unnecessary costs and lost productivity in the workplace, not to mention the risk to an employee’s health. By giving care providers access to relevant medical prescription histories, they can eliminate the potential disconnect in care and empower them to make more informed and effective decisions.
Further, insight from other providers can help with early detection of issues not caught in routine screenings. For example, if an optometrist discovers retinal bleeding, they can flag this information for the patient’s primary care provider to follow up with a diabetes evaluation.
Recently, a Deloitte research report showed that the American corporate wellness market — which includes healthcare — is one of employers’ top concerns and is already worth more than $8 billion. This market is expected to continue to grow as wellness is projected to reach over $11 billion by 2021. To help curtail these costs, employers should be offering integrated benefits solutions that place a premium on the whole employee’s health with the knowledge that it will benefit the organization in the end.
By providing each of your employees’ medical practitioners with complete pictures of their health, you can address these challenges, reduce health care costs for your business, improve the treatment your employees receive and in turn, increase your business’s productivity and bottom line. After all, the various systems within the human body are interconnected, so shouldn’t our healthcare reflect that, too?