You’ve likely heard of at least one direct-to-consumer genetic test on the market — yes, those tests that tell you about your ancestry and health risks by analyzing your DNA — and for good reason. MIT Technology Review reported that 2017 was the year “
Why should you start paying attention? Maybe genetic testing and screening became an afterthought to you upon the passing of the
Well, it’s time to get up to speed, as genetic testing and screening services are starting to become mainstream, and you’re highly likely to have a vendor in this space knock on your door soon to tout the benefits of what they are selling. As examples, Color Genomics has a number of employer
1. You’re already paying for genetic testing.
Take a closer look at your health plan’s medical policy and you’ll find that it is already covering a host of genetic tests, including gene analysis of the BRCA 1 and 2 for breast cancer, cystic fibrosis and Down syndrome. It’s important that employers ask questions about how health plans are making decisions about this type of benefits coverage, especially as the technologies available rapidly evolve. Have you seen data from your health plan or data warehouse on what you’ve paid for genetic tests? You may be surprised by the amount you’re already paying for genetic testing and/or the cost increase year-over-year.
2. New tests are popping up daily.
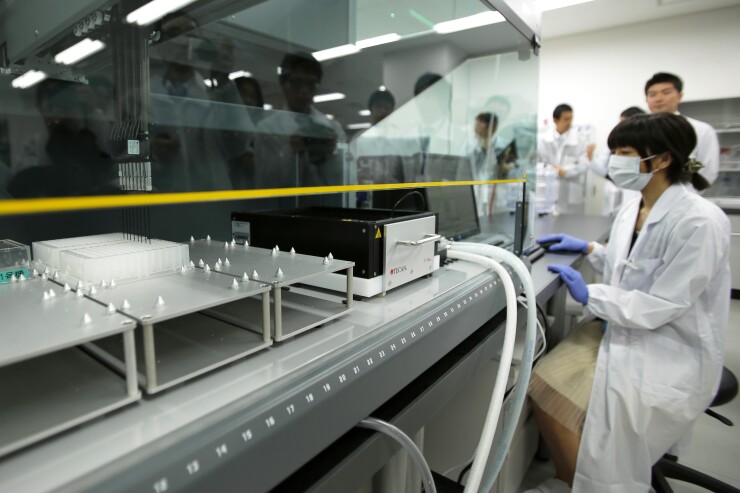
Genetics is truly the Wild West in healthcare. Only in 2003 was the entire human genome mapped. Today, there are over 75,000 genetic tests on the market and
· How do you evaluate from a clinical perspective which genetic tests to cover? Do you evaluate whether the presence of the gene or panel is proven to be scientifically linked to a diagnosis or treatment decision?
· What are the lab certifications and provider qualifications for those who provide the analysis and interpretation?
· What is the expected hard return on investment (ROI) in the program?
· What is the expected soft ROI, e.g., members are more engaged in their health and
· It’s important that employers understand how to discern which services deliver incremental value over the status quo.
3. There are opportunities to implement controls.
Employers have seen the costs of genetic tests paid through their health plan well exceed trend. Why? In some cases, the test clearly fits into one category, e.g., breast cancer, hereditary cancers or prenatal. In others, the test falls into an “unspecified” or “other” category. For an employer to uncover these tests, require digging deeper into the data and discussing opportunities to implement controls. For example, a utilization management program could control for the tests that fall into this black box or are particularly high-cost. It also could narrow the laboratory network that conducts the testing, which presents an opportunity to manage future cost and utilization increases.
4. You’ll have a steeper learning curve later.
With all the tests on the market, the continued explosion of new tests entering the market, and the continued advancements in genetics, it’s time to start getting a handle on this space now. You can start by taking the following steps:
· Ask your health plan to report to you on the spending and utilization for genetic testing over the last few years.
· Get an overview of your health plan’s medical policy and how it stays current on this quickly developing area.
· Understand the coverage for genetic tests under your current benefit design.
· Learn how your health plan manages its network of laboratories.
· Finally, determine the level of support your members can receive from genetic counselors or others, whether through your health plan or other vendors.
· Learning about genetic testing today will prepare you for a future where it’s guaranteed to factor more largely in healthcare.





