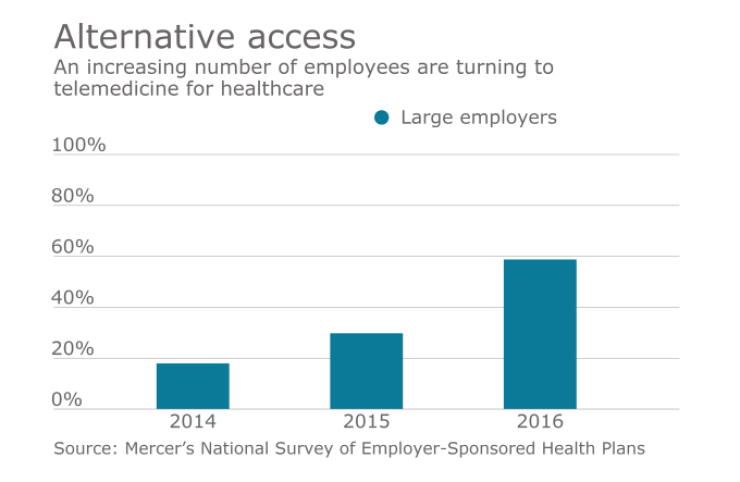
Most employers today are adding telemedicine to their health benefits package in an effort to reduce costs and improve access to care. The thinking is, having a provider at the employee’s fingertips can reduce unnecessary (and expensive) urgent care or ER visits and encourage time-challenged employees to seek medical advice sooner, before a condition becomes more serious.
And yet, while the potential for telemedicine is high, utilization remains low. In fact, just 7% of employees with telemedicine access use it, according to the 2015 Willis Towers Watson/NBGH “Best Practices in Healthcare Employer Survey.”
So why aren’t employees using telemedicine services that are freely available to them?
I don’t think it’s about the technology; I think it’s about wanting a connection with our doctors.
In fact, more than half of 1,500 full-time professionals across the United States say they would be more likely to use a telemedicine service if it were offered by their healthcare provider, according to a survey conducted by One Medical Group, a concierge medical practice.
See also:
This stat doesn’t surprise me at all. Think about it: Most of us don’t want to see just any old doctor. We want to research the practice on Yelp and make sure the providers are high-quality, or ask our friends for recommendations. We want to build a relationship. We want to feel trust.
The doctor on the other end of most telemedicine calls doesn’t know us. She probably also doesn’t have our full health record. Heck, she might not even be employed by the provider.
Who is she? It sure is hard to trust someone you don’t know.
See also:
That’s why telemedicine that’s integrated with our existing primary care — where telemedicine services are offered by our doctor’s office or primary care practice — is a lot more likely to be trusted and used than standalone options.
When the provider that picks up the call is part of your doctor’s office, they have access to your full visit history. They know if you’re dealing with chronic back pain or urinary tract infections. They can see that you’re prone to ear infections or coping with anxiety. They’re a part of your team.
They know you.
But it’s not just about trust — it’s also about continuity of care.
While standalone telemedicine can be very effective for a particular set of conditions, one of the challenges with stand-alone telemedicine apps is that if the issue can’t be resolved via telemedicine, patients may end up with a more fragmented healthcare experience.
What happens when the ear infection doesn’t go away? Or I have a bad reaction to a medication? What’s my next step?
See also:
Telemedicine that is offered by our primary care provider is just the first step in a comprehensive care path. We know that if our problem can’t be solved remotely, or we need follow-up, we can come into the office for an in-person visit. All the information from the virtual visit will already be in our record — no need to start over again.
We’re just in the initial innings when it comes to telemedicine’s ability to transform care. While the gains we’ve made from greater availability of telemedicine have been powerful, fundamentally transforming care through telemedicine will require integrating it more thoroughly into our care delivery system.





